Perfect bilateral body symmetry is more of a theoretic concept that seldom exists in living organisms. However, pronounced and recognizable face asymmetries do exist and can have serious esthetic, functional and psychological implications.
Asymmetry in the craniofacial areas may be the result of discrepancies either in the form and/or size of individual bones as well as malposition of one or more bones in the craniofacial complex. The asymmetry may also be limited to the overlying soft tissues (1). Early detection of face asymmetry may be critical with regard to the diagnosis, prognosis, and therapeutic management. The aim of this article is to briefly present the major categories of face asymmetries in children and adolescents and to provide information on their clinical characteristics.
Etiology
Genetics have been implicated in certain conditions such as multiple neurofibromatosis (Figure 1), hemifacial microsomia, cleft lip and palate.
Intrauterine pressure during pregnancy and significant pressure at the birth canal during parturition can have observable effects on the bone of the fetal skull.
Environmental factors can cause face asymmetry and may include pathological changes that are not congenital in nature (e.g., osteochondroma of the mandibular condyle), trauma, infection and inflammation within the temporomandibular joint (TMJ), ankylosis of the mandibular condyle to the temporal bone, damage to a nerve, which may indirectly lead to asymmetry from the loss of muscle function and tone, and sucking or chewing habits with influence on tooth position equilibrium (1,2).
Classification Skeletal Asymmetries
The skeletal asymmetries may involve one bone (e.g., maxilla or mandible) or a number of skeletal and muscular structures on one side of the face.
Hemifacial microsomia
Hemifacial microsomia results from the malformation of the 1st and 2nd branchial arches. Involves mostly unilateral condylar underdevelopment, it may be associated with variable abnormalities of the external and middle ear, has similar manifestations with Goldenhar syndrome, and its etiology is heterogeneous. The extent of TMJ involvement primarily determines severity, prognosis, timing and type of treatment. Face asymmetry in hemifacial microsomia is characterized by chin deviation. Occlusal manifestations include lower dental midline deviation, unilateral cross bite, tilting of the occlusal plane, all of them towards the affected side (Figure 2). Apart from ear abnormalities, soft tissue defects may include skin tags, facial clefts, cranial nerve function, soft palate function, bulk of subcutaneous soft tissue, muscles of mastication and facial expression, macrostomia, and skin tags (3).
Hemimandibular hyperplasia
Hemimandibular hyperplasia is an uncommon maxillofacial deformity characterized by increased ramus height, rotated facial appearance, and kinking at the mandibular symphysis. Usually it is associated with prominence of the lower border of the mandible, maxillary and mandibular alveolar bone overgrowth, compensatory canting of occlusal plane, and serious functional malocclusion (4) (Figure 3). Heminandibular hyperplasia presents diffuse enlargement of the condyle, the condylar neck, the ramus, and the body of the mandible, it usually begins before puberty, is clearly due to hyperactivity in the condyle, whose cartilage actively proliferates.
Figure 1. Facial photograph of an 11-year-old girl with neurofibromatosis (a). The lesion is also apparent in lateral cephalometric (b) and panoramic (c) radiographs.
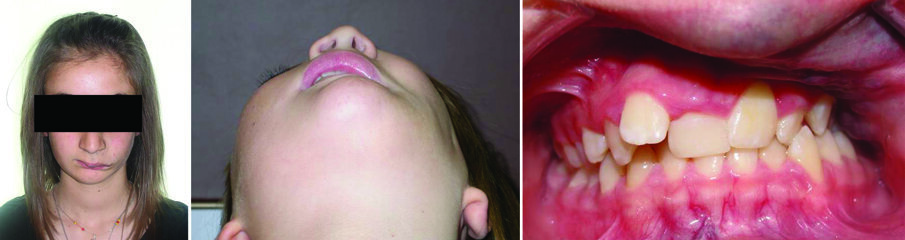
Figure 2. Facial photograph of a 13-year-old girl with hemifacial microsomia (right side) (a). The discrepancies include asymmetries in the mandibular body, ramus, and condyle, as well as involvement of the ear. Malocclusion is characterized by right posterior crossbite, tilting of the occlusal plane and lower dental midline deviation to the affected side (b).
Figure 3. Facial photograph of a 16-year-old girl with heminandibular hyperplasia (right side). The discrepancies include asymmetries in the mandibular body, ramus, and condyle (a). Malocclusion is characterized by left anterior crossbite and lower dental midline deviation to the non-affected side (b).
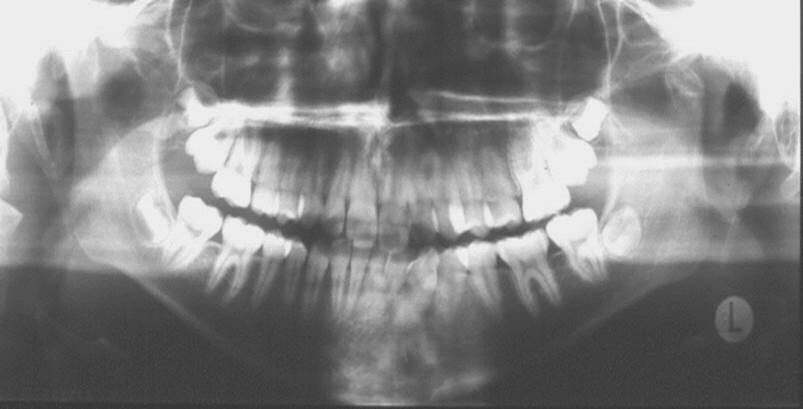
Figure 4. Panoramic radiograph of a 15-year-old girl showing fracture of the left condyle.
Figure 6. A 10-year-old boy with dermatomyositis creating a soft tissue tonicity imbalance (a) and resulting in a unilateral posterior crossbite (b).
Figure 5. Facial photograph of a 16-year-old boy with osseous ankylosis of the left TMJ. The discrepancies include severe asymmetries in the mandibular body and ramus (a). Malocclusion is characterized by left anterior and posterior crossbite, tilting of the occlusal plane, and lower dental midline deviation to the affected side (b).
Figure 7. A 13-year-old girl with hemangioma “infrabulbare” (a) applying excessive pressure on the left maxillary teeth (b) and severely influencing their position (c).
Condylar fracture
Condylar fractures in growing individuals are usually the results of accidents and sports (Figure 4). In children they are often overlooked by parents and physicians since short time after the injury symptoms of pain usually disappear. The majority of condylar fractures in children, if properly diagnosed and managed by short-term intermaxillary fixation and subsequent physiotherapy, do not lead to morphological and functional problems. However, no diagnosis of condyle fractures may lead to face asymmetries, severe malocclusion and TMJ ankylosis (5).
TMJ ankylosis
It is a chronic hypomobility and, if happens in growing subjects, it becomes a growth disorder (Figure 5). It results from intracapsular adhesions or ossification between the disc and temporal articular surface that attach the disc-condyle complex to the articular eminence. Its classification relates to the degree of limitation (partial or complete), location of the union (intracapsular vs. extracapsular), and type of tissues involved (fibrous, osseous, fibro-osseous). TMJ ankylosis occurs relatively infrequently. Principle causes include trauma, previous joint surgery, systemic or local infections, tumors, compressive function pattern and systemic diseases (6). Regarding history, patients report limited mouth opening without any pain, the condition has been present for a long time, and, if not associated with severe dentofacial deformity, patients do not feel that it poses a significant problem.
Muscular and Soft Tissue Asymmetries
Facial disproportions could be the result of muscular and soft tissue asymmetry (e.g., hemifacial atrophy or cerebral palsy), muscle size disproportion in volume and/or tonicity (e.g., masseter hypertrophy, dermatomyositis (Figure 6), and neoplasms (Figure 7)). Abnormal muscle function often leads to skeletal deviations (2).
Functional Asymmetries
Functional asymmetries can result from lateral or anteroposterior deflections of the mandible due to occlusal interferences, which prevent proper intercuspation in centric relation (e.g., functional crossbites) (1). Functional crossbites in children, if left without correction, subsequently they may cause mandibular asymmetry.
Conclussions
Face asymmetries in children and adolescents should be detected and diagnosed as early as possible. Early detection may be critical with regard to the prognosis and therapeutic management of this challenging dentofacial deformity.
References
1) Bishara SE, Burkey PS, Kharouf JG, Athanasiou AE. Dental and facial asymmetries. In: Bishara SE, ed. Textbook of Orthodontics. Philadelphia: WB Saunders Company, 2001:532-44.
2) Melsen B, Athanasiou AE. Soft Tissue Influence in the Development of Malocclusion. Aarhus: The Royal Dental College, 1987.
3) Assael LA. Developmental disorders. In: Kaplan AS, Assael LA, eds. Temporomandibular Disorders. Diagnosis and Treatment. Philadelphia: WB Saunders Company, 1991:238-250.
4) Obwegeser HL. Mandibular Growth Anomalies. Berlin: Springer, 2001:145-194.
5) Myall RW, Sandor GK, Gregory CE. Are you overlooking fractures of the mandibular condyle? Pediatrics 1987;79:639-41.
6) Vasconcelos BC, Porto GG, Bessa-Nogueira RV. Temporomandibular joint ankylosis. Braz J Otorhinolaryngol 2008;74:34-8.
Align Technology, Inc. (NASDAQ: ALGN) today introduced the latest version of its proprietary ClinCheck treatment planning software. ClinCheck software ...
Dental Tribune MEA had the pleasure to interview Markus Sebastian, SVP and MD of Align Technology EMEA, during his recent visit to Dubai, United Arab ...
Dental Tribune Middle East had the pleasure of speaking with Dr Rafif Tayara, a distinguished consultant pediatric dentist with a passion for holistic care,...
Dental Tribune talks with Kirill Levin, Group Vice President of the Eastern Group Regional Commercial Organization (RCO) at Dentsply Sirona, about key ...
Oral health has been a top priority in the Dubai Health Authority agenda for the strategy 2021. The main aim is to decrease the level of caries for children...
LEIPZIG, Germany: A recent expert review has set out evidence-based consensus recommendations to help dental teams in the Middle East and Africa (MEA) ...
AMMAN, Jordan: Dental and facial aesthetics do more than shape a smile; they can influence how individuals perform socially and academically, according to ...
DOHA, Qatar: Virtual reality (VR) is rapidly gaining ground in dental training, particularly for restorative dentistry. A new bibliometric study from a team...
Removable prosthetics as high-quality restorative treatment in the edentulous patient
Live webinar
Tue. 24 February 2026
10:00 pm UAE (Dubai)
Prof. Dr. Markus B. Hürzeler
Live webinar
Wed. 25 February 2026
12:00 am UAE (Dubai)
Prof. Dr. Marcel A. Wainwright DDS, PhD
Live webinar
Wed. 25 February 2026
8:00 pm UAE (Dubai)
Prof. Dr. Daniel Edelhoff
Live webinar
Wed. 25 February 2026
10:00 pm UAE (Dubai)
Live webinar
Thu. 26 February 2026
5:00 am UAE (Dubai)
Live webinar
Tue. 3 March 2026
8:00 pm UAE (Dubai)
Dr. Omar Lugo Cirujano Maxilofacial
Live webinar
Wed. 4 March 2026
5:00 am UAE (Dubai)
Dr. Vasiliki Maseli DDS, MS, EdM



 Austria / Österreich
Austria / Österreich
 Bosnia and Herzegovina / Босна и Херцеговина
Bosnia and Herzegovina / Босна и Херцеговина
 Bulgaria / България
Bulgaria / България
 Croatia / Hrvatska
Croatia / Hrvatska
 Czech Republic & Slovakia / Česká republika & Slovensko
Czech Republic & Slovakia / Česká republika & Slovensko
 France / France
France / France
 Germany / Deutschland
Germany / Deutschland
 Greece / ΕΛΛΑΔΑ
Greece / ΕΛΛΑΔΑ
 Hungary / Hungary
Hungary / Hungary
 Italy / Italia
Italy / Italia
 Netherlands / Nederland
Netherlands / Nederland
 Nordic / Nordic
Nordic / Nordic
 Poland / Polska
Poland / Polska
 Portugal / Portugal
Portugal / Portugal
 Romania & Moldova / România & Moldova
Romania & Moldova / România & Moldova
 Slovenia / Slovenija
Slovenia / Slovenija
 Serbia & Montenegro / Србија и Црна Гора
Serbia & Montenegro / Србија и Црна Гора
 Spain / España
Spain / España
 Switzerland / Schweiz
Switzerland / Schweiz
 Turkey / Türkiye
Turkey / Türkiye
 UK & Ireland / UK & Ireland
UK & Ireland / UK & Ireland
 International / International
International / International
 Brazil / Brasil
Brazil / Brasil
 Canada / Canada
Canada / Canada
 Latin America / Latinoamérica
Latin America / Latinoamérica
 USA / USA
USA / USA
 China / 中国
China / 中国
 India / भारत गणराज्य
India / भारत गणराज्य
 Pakistan / Pākistān
Pakistan / Pākistān
 Vietnam / Việt Nam
Vietnam / Việt Nam
 ASEAN / ASEAN
ASEAN / ASEAN
 Israel / מְדִינַת יִשְׂרָאֵל
Israel / מְדִינַת יִשְׂרָאֵל
 Algeria, Morocco & Tunisia / الجزائر والمغرب وتونس
Algeria, Morocco & Tunisia / الجزائر والمغرب وتونس



























































To post a reply please login or register